by hanna | Jan 6, 2021 | General News, Physical Health
Coronavirus cases have been spreading in the United States since early 2020 and cases have been on the rise since the fall months. Becoming informed and taking proper precautions is imperative in beating this disease. Basic Facts What is COVID-19? COVID-19 is a...

by hanna | Jan 6, 2021 | Nutrition, Physical Health
Did you know that sugar is the most popular ingredient added to foods in the United States? In fact, the average American consumes 152 pounds per year—that’s three pounds per week! Serious health complications can arise when too much sugar is consumed including weight...

by hanna | Oct 29, 2020 | Events, General News
November flu shot clinic open to adult DFD patients DFD Russell Medical Centers is offering a free flu clinic for its patients on Saturday, November 7 from 10am-2pm at our Monmouth, Turner and Leeds locations. Getting a flu shot lowers your risk of contracting the...

by hanna | Aug 18, 2020 | Physical Health
Lying on the beach or by the pool is relaxing, but water can also be a great tool to implement into your workout routine. Exercising in water provides the resistance needed to strengthen muscles while also relieving joints of high impact pressure of other exercises....

by hanna | Aug 13, 2020 | General News, Nutrition, Physical Health
Now Open for Registration! DFD Russell Medical Centers is excited to announce new workshops by Healthy Living for Me. These workshops each discuss one topic including Living Well for Better Health, Living with Chronic Pain and Living with Diabetes. Healthy...
by hanna | Jun 8, 2020 | General News
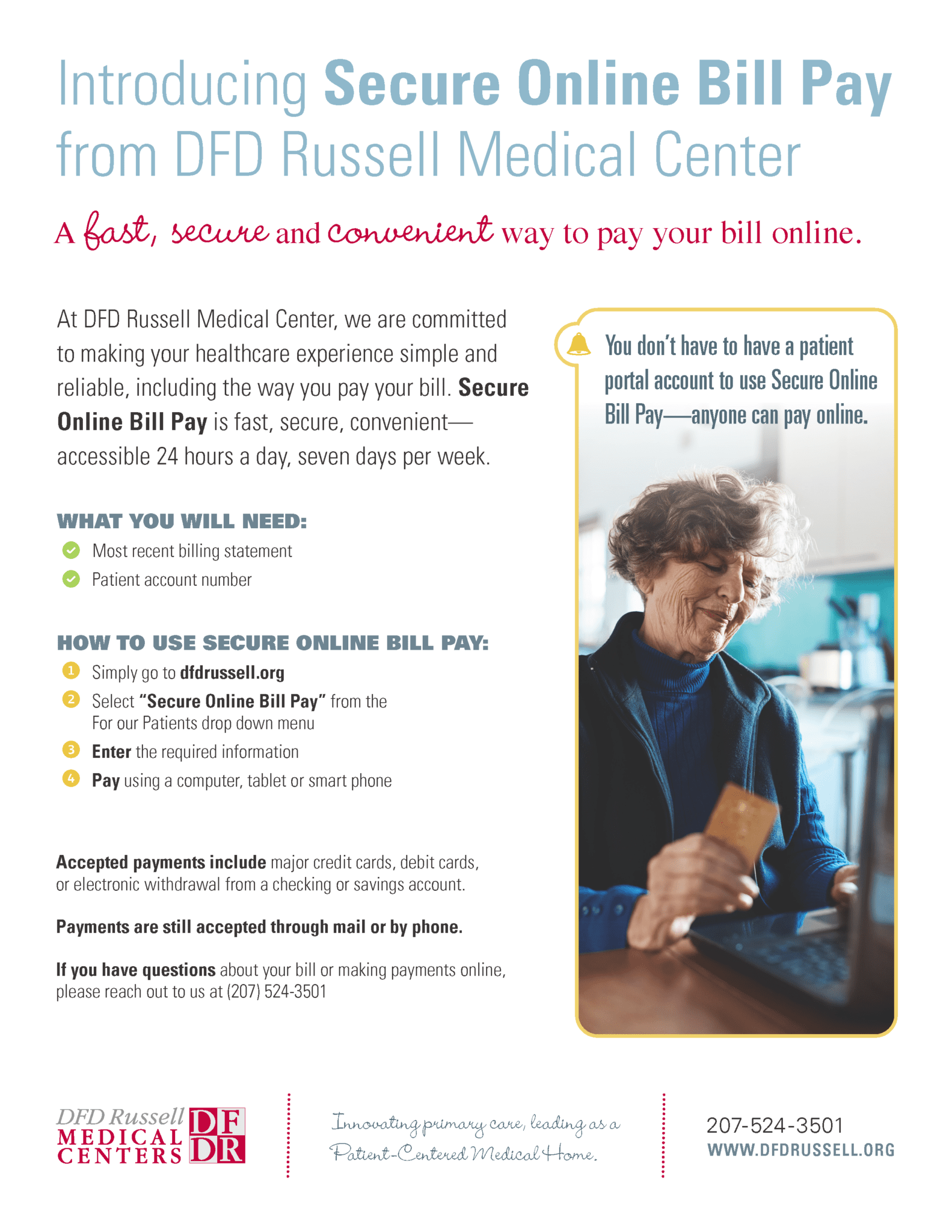
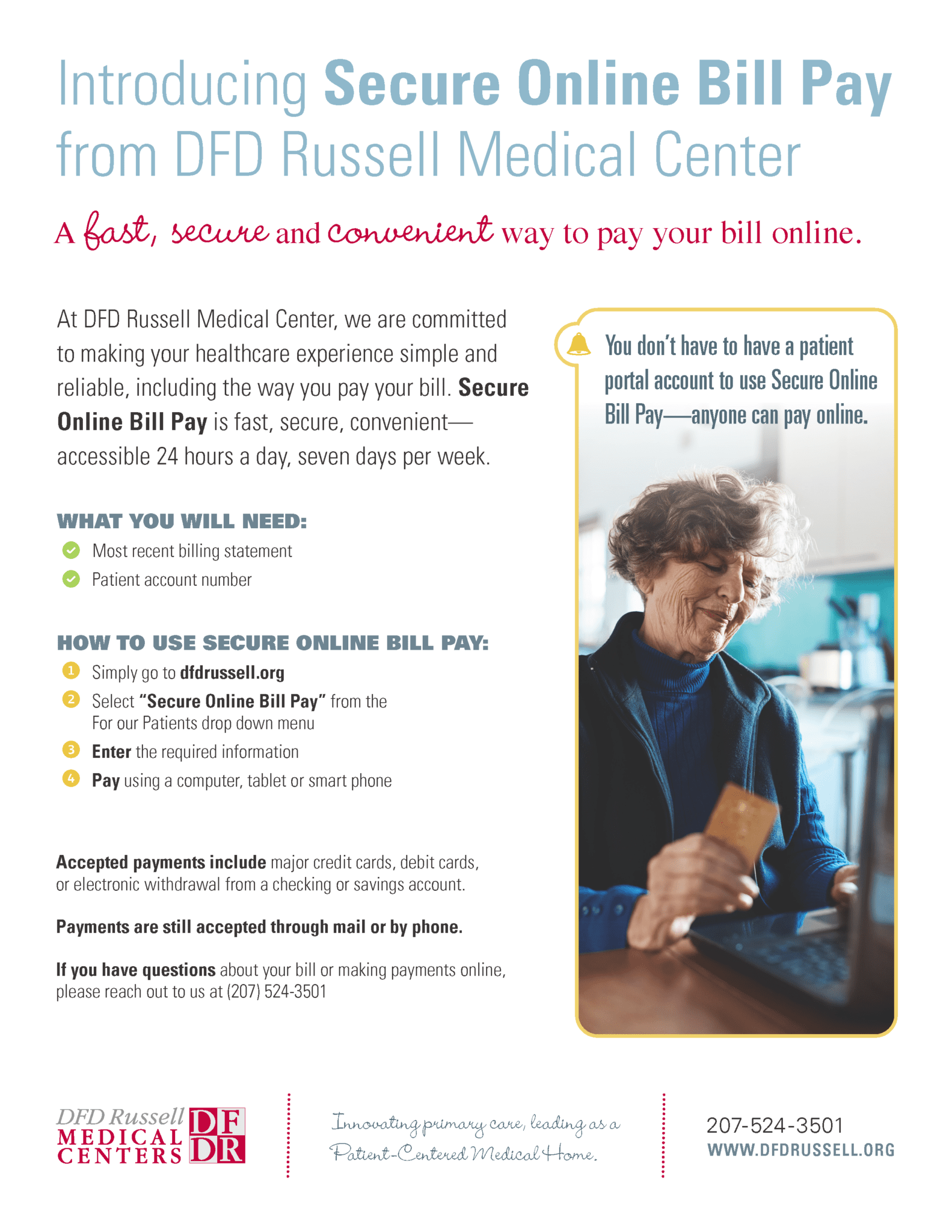
A fast, secure and convenient way to pay your bill online. At DFD Russell Medical Center, we are committed to making your healthcare experience simple and reliable, including the way you pay your bill. Secure Online Bill Pay is fast, convenient and accessible 24 hours...
by hanna | Apr 28, 2020 | General News
Mental health is your emotional, psychological and overall wellbeing. It affects how you think, feel and act. It also helps in establishing how you handle stress, relate to other people, and make choices. Your mental health is not in a static state and requires your...
by jennie | Mar 21, 2020 | General News
The health and safety of our patients, staff, and community are of the highest priority to DFD Russell Medical Centers. We are committed to taking all necessary precautions to actively reduce the risk of further transmission of COVID-19 in our community. Please...

by hanna | Mar 20, 2020 | Mental Health, Nutrition, Physical Health
In times of high stress and uncertainty, it’s easy to let our routines and healthy habits fall to the wayside. But if we let anxiety and stress overwhelm us, our health could suffer. This is the opposite of what your body and mind need! Let’s talk about some easy ways...

by hanna | Feb 24, 2020 | Nutrition
Nutrition—what does it actually mean? Yes, nutrition is the biological process of providing your body with proper foods for growth and function, but it’s also more than that. Nutrition is about making informed decisions to better your physical, mental and emotional...